Congratulations ! If you’re like me you are one of the 30 million adults in the United States who suffer with joint pain, you know the pain often is debilitating. It can keep you from staying active and limits your mobility and it even makes daily chores seem impossible. What you might not know is that many doctors can treat joint pain with more than just pills or surgery. Beware though some doctors will tell you about one procedure and then change it once they know your insurance example Medicare I felt one doctor thought less of me as a patient because I am disabled so he changed or tried to change the procedure. It pissed me off because I was all set to get the procedure we discussed and then he changed it.
Both procedures were covered under Medicare so I felt betrayed as if I wasn’t good enough for the other injection.
Newsflash …..people on Medicare pay for the insurance they have. It’s not free , hell I pay more for insurance than when I was working.
But thankfully Medicare is good coverage. Low deductible.
It’s some doctors that treat you like a second class citizen.
Make sure this doesn’t happen to you.
Depending on the severity of your pain, injections can be another option for easing your joint pain and help to get you moving again.
Doctors use these injections to try to reduce inflammation and pain in your joints some come with side effects and some risks.
The injections range from corticosteroids, which have been around for decades, to newer ortho-biologic injections like platelet-rich plasma (PRP) , Stem Cell and placental tissue matrix (PTM)
You and your physician will decide which one is best based on your individual needs. The issue is finding doctors qualified to do these.
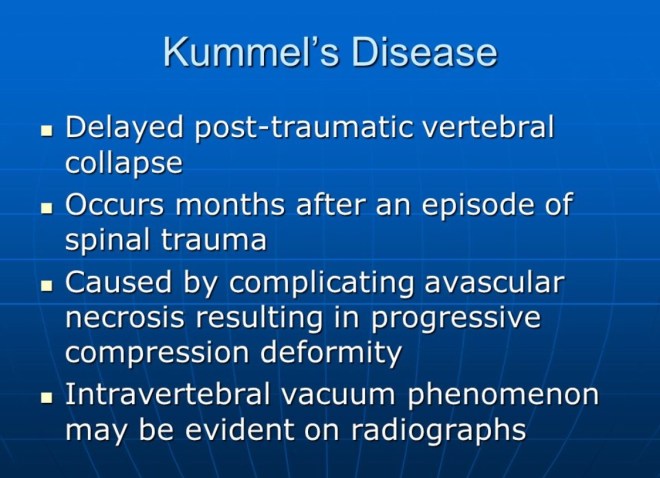
Not every injection is right for every patient, in my case I hate steroid injections, not only did it make my pain worse it also comes with the risk of developing osteonecrosis. Something I already have. I have noticed that it seems like doctors are quick to prescribe and inject steroids. I stand my ground and refuse. But that’s me.
So here are some facts to help you know more about the options.
Corticosteroid injections
Use: This injection is the first line of defense against osteoarthritis symptoms and other joint pain in shoulders, knees and hips. Corticosteroids can offer relief for two to three months, and reduce inflammatory cell activity in the joint. In some people.
Side effects and Risks : As with all injections, there’s a small chance of infection about one in 1,000 as well as Joint infection.
Nerve damage.
Thinning of skin and soft tissue around the injection site.
Temporary flare of pain and inflammation in the joint.
Tendon weakening or rupture.
Thinning of nearby bone (osteoporosis)
Osteonecrosis lack of blood supply to the bone
Raised blood sugar level
Whitening or lightening of the skin around the injection site
Cost: Most insurance covers the $100 -$200 usd cost of these injections. Your insurance provider may require that you try at least one corticosteroid injection first to see whether it works. If not, you may move on to a different therapy.
Hyaluronic acid injections
Use: Hyaluronic acid (HA) injections often are used when corticosteroid injections don’t work. But they usually are approved only for use in the knee.
In some instances, doctors consider an HA injection first if you don’t have obvious signs of inflammation. HA also is a better option if you have diabetes, as corticosteroids can raise blood sugar levels.
Also known as gel injections, HA injections are chemically similar to your natural joint fluid.
When you have osteoarthritis which is different than osteonecrosis lucky me I have both, the joint fluid becomes watery.
So, this injection helps to restore the fluid’s natural properties and works as a lubricant and a shock absorber.
HA is a cushion or a buffer against inflammatory cells in the joint. In some cases, it can stimulate the knee to start producing more natural HA.” Some physicians also believe that HA helps reduce pain by coating nerve endings within the joint.
One treatment, which may consist of between one and three injections, usually offers symptom relief for four to five months, but sometimes up to one years. However, pain and stiffness will return. Most insurance companies only approve one HA injection every six months.
In knees with osteoarthritis, the joint fluid (called synovial fluid) can break down and not provide the cushioning your knee needs
Durolane
Euflexxa
Hyalgan
Orthovisc
Monovisc
Supartz
Synvisc, Synvisc-One
Depending on which type your doctor uses, you may get a single shot. Or you’ll get three to five injections spaced a week apart.
Side effects: There’s a 1-in-100 chance of an inflammatory reaction, The most common short-term side effects are minor pain at the injection site and minor buildup of joint fluid. These get better within a few days.
Cost: HA injections cost more — about $300 to $850 per injection, but most insurance companies cover the cost for knee injections.
Platelet-rich plasma (PRP) injections
Use: Platelet-rich plasma (PRP) injections can treat osteoarthritis joint pain, and are being thoroughly researched to understand their effects.
These injections use your own blood and platelets to promote healing. Platelets contain growth factors and proteins that aid healing in soft tissues. Research shows PRP injections can alter the immune response to help reduce inflammation,
Side effects: Side effects include a very low risk of infection and pain at the injection site. You must stop oral anti-inflammatory medications for a short amount of time if you get a PRP injection.
Cost: Insurance companies don’t generally cover PRP injections and you will pay between $400 and $1,300 per injection out-of-pocket.
Stem Cell Injections
The world’s most advanced regenerative injection treatments for treating knee pain due to arthritis, meniscus tears, traumatic ligament injuries, overuse conditions and other degenerative conditions.
Side effects : mild discomfort associated with the procedure. There is a very small risk of infection whenever aspirations and injections are performed. Nerve damage, vessel damage, and injury to other important structures are exceedingly rare
Placental tissue matrix (PTM) injections
Use: Placental Tissue Matrix (PTM) injections can very profoundly decrease the pain related to osteoarthritis.
These are injections of placental tissue, which is obtained after a healthy baby is delivered from a healthy mother. Research has discovered that there is a large number of growth factors in placental tissue that promote healing, Dr. Genin says.
Side effects: Side effects include a low risk of infection and pain at the injection site. The placental tissue is “immune privileged,” which means the body would not have an adverse reaction to it.
Cost: Insurance companies don’t generally cover PTM injections; you will pay around $1,800 -$2500 per injection out-of-pocket.
Many of these injections often are effective in reducing or stopping your joint pain, but it’s important to remember that they may not keep the pain from returning, Dr. Schaefer says. In fact, they’re most effective when used with other therapies.
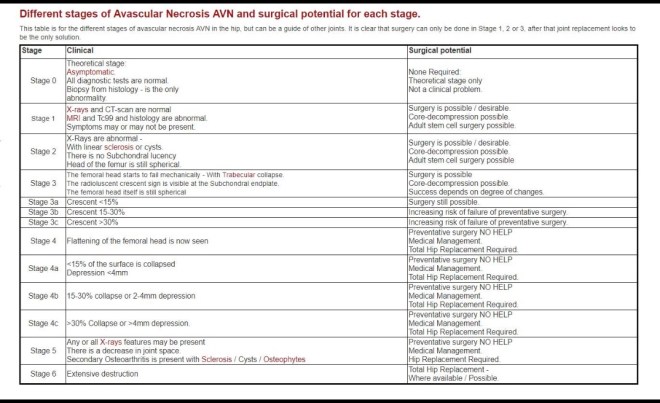
As a patient who has Osteonecrosis, Osteoarthritis, and other stuff I consider surgical options as a last resort only if other treatment options have failed. Unfortunately some treatments I cannot even afford to try. I wish the FDA would get a move on and approve some things so insurance companies can have this as a form of treatment.
Stem Cells
BONE MARROW AND FAT CELLS
The stem cells used in this point of care clinic are Autologous Cells that we take from your own body. These cells are taken from your own Bone Marrow or Fat Cells. The cells are your own Stem Cells and will not be rejected by your body.
Taking the Bone Marrow or Fat Cells from your body is relatively painless as a mild local anesthetic is used prior to harvesting. These cells are processed to receive the most stem cell gain and then injected into the area of your body where you need the growth factors to go to work the quickest. Your blood is also drawn and your platelet rich plasma is added to the Stem Cells taken from your Bone Marrow or Fat Cells to increase the activity of the growth factors.
It is important that these cells are used the day they are extracted from your body in order to insure they remain alive and active. Our clinic does not grow extra stem cells from your Bone Marrow or Fat Cells to ensure that they are alive and active. It is an FDA requirement that you receive your cells the same day they are harvested.
You get only the stem cells we extract from your body and there is no other manipulation used except extraction and preparation of the samples taken from your own body. The cells are taken in a procedure that creates only mild discomfort or none at all. Ninety nine percent of our patients experience no pain obtaining bone marrow or fat cells.
CORD STEM CELLS:
Embryo and Placenta stem cells can create certain types of cancers. The cord blood Stem Cells should only be used if they are obtained from a healthy relative and you are a good match. Cord Stem Cells that are used outside of the country or shipped to this country are illegal. The FDA has found diseases in these grown cells and states that most of them are dead. Even though the physicians supplying these Cord Cells claim they are safe to use, you should use extreme caution before considering these procedures.
ARE YOU A CANDIDATE FOR THESE STEM CELL PROCEDURES
REBUILDING JOINTS & SPINE: The Stem Cells that are obtained from your body are placed into all joints and spine to rebuild and regenerate new tissue growth as determined by the clinic physician. There has been clinical evidence that new cartilage can be grown within your joint provided you are determined a candidate by the clinical physician. Not all patients will be a candidate and may require joint replacement.
TORN TENDONS: If the patients tendons are not completely torn this procedure will produce new tissue growth to regenerate torn tendons. Our clinic physician can only determine this with an initial visit and evaluation.
How Does PRP Therapy Work?
To prepare PRP, a small amount of blood is taken from the patient. The blood is then placed in a centrifuge. The centrifuge spins and through a multi-functional process separates the plasma from the blood producing the PRP. This increases the concentration of platelets and growth factors up to 500% also increasing hMSC (human stem cells) proliferation as a function of 8-day exposure to platelet released concentrations 10x. (x= increase above native levels)
When PRP is injected into the damaged area it stimulates the tendon or ligament causing mild inflammation that triggers the healing cascade. As a result new collagen begins to develop. As this collagen matures it begins to shrink causing the tightening and strengthening of the tendons and ligaments of the damaged area.
What is Platelet Rich Plasma?
Platelet Rich Plasma or PRP is blood plasma with concentrated platelets. The concentrated platelets found in PRP include growth factors among the huge reservoirs of bioactive proteins that are vital to initiate and accelerate tissue repair and regeneration. These bioactive proteins increase stem cell production to initiate connective tissue healing, bone regeneration and repair, promote development of new blood vessels and stimulate the wound healing process.
PRP Regenerates Tendons & Ligaments
Tendons connect the muscle to the bone making it possible for you to do many everyday physical activities. Overuse or damage to the tendon over a long period of time causes the collagen fibers in the tendons to form small tears, a condition called tendonitis. Damage to tendons most often occurs in the knees, ankles, hips, spine, elbows, shoulders, and wrists.
Ligaments are composed of collagen fibers that hold one bone to another, stabilizing the joint and controlling the range of motion. When a ligament is damaged, it is no longer able to support the bones in the joint, which often leads to pain symptoms. The instability causing the pain in your joints does not always show up on high tech imaging equipment. Through a thorough neurological and orthopedic evaluation Dr. Baum can determine which ligaments and tendons are unstable due to injury, wear or tear.
Tendons and ligaments have a poor blood supply and they do not usually heal from damage. Combined with the stress of day-to-day activities tendons and ligaments become inefficient causing degeneration of the joint which leads to chronic pain and weakness. Patients who experience chronic pain may not even remember when the injury occurred.
How Does PRP Compare With Cortisone Shots?
Studies have shown that cortisone injections may actually weaken tissue. Cortisone shots may provide temporary relief and stop inflammation, but may not provide long term healing. PRP therapy is healing and strengthening these tendons and ligaments and in some cases thickening the tissue up to 40%.
Treatment Plan
PRP injections with guided ultrasound can be performed on tendons and ligaments all over the body. Cervical, thoracic and lumbar spine, degenerative disc disease, arthritic joints shoulder pain, hip pain, and knee pain, even the smaller joints of the body can all be treated effectively with PRP. Dr. Baum will determine whether prolo solution, Platelet Rich Plasma or a combination of both will be the most effective form of treatment for you during his initial consult and evaluation.
Frequency Of Treatments
While responses to treatment vary, most people will require 3 to 6 sets of injections of PRP. Each set of treatments is spaced 4 to 6 weeks apart.
Is PRP Right For Me?
If you have degenerative spine or joint disease, a tendon or ligament injury, laxity or tear and traditional methods have not provided relief then PRP therapy may be the solution. It will heal tissue with minimal or no scarring and alleviates further degeneration and builds new tissues. There will be an initial evaluation with Dr. Baum to see if PRP therapy is right for you.
What Can Be Treated?
Platelet Rich Plasma injections helps regenerate all areas of the body including the cervical, thoracic and lumbar spine, wrists, elbows, shoulders, hips, knees and ankles as well as tendons and ligaments all over the body. Dr. Baum is one of the few physicians performing PRP procedures to all areas of the spine. Our clinic treats patients with sports injuries, arthritic and degenerative joints and degenerative disc disease. More specific injuries including tennis elbow, carpal tunnel syndrome, scoliosis, ACL tears, shin splints, rotator cuff tears, plantar faciitis and iliotibial band syndrome may all be effectively treated with PRP.
What Are The Potential Benefits?
Patients can see a significant improvement in symptoms as well as a remarkable return of function. This may eliminate the need for more aggressive treatments such as long-term medication or surgery.
Special Instructions
You are restricted from the use of non-steroid anti-inflammatory medications (NSAIDs) one week prior to the procedure and throughout the course of treatments.
Initially the procedure may cause some localized soreness and discomfort. Most patients only require some extra-strength Tylenol to help with the pain. Ice and heat may be applied to the area as needed.
How Soon Can I Go Back Regular Activities?
PRP therapy helps regenerate tendons and ligaments but it is not a quick fix. This therapy is stimulating the growth of new tissue requiring time and rehabilitation. Under Dr. Baum’s supervision patients will begin an exercise program immediately following the first procedure. During the treatment program most people are able to resume normal activities and exercise.
Platelet Rich Plasma (PRP) Matrix Graft by David Crane, MD and Peter A.M. Everts PhD
PRP application techniques in musculoskeletal medicine utilize the concentrated healing components of a patient’s own blood—reintroduced into a specific site—to regenerate tissue and speed the healing process
PRP INJECTION APPLICATION SITES
Spine
Cervical/Thoracic/Lumbar/Sacral
Shoulders & Elbows
Wrist & Hand
Hip/Pelvis
Knee & Lower Leg
Ankle & Foot
Fingers & Toes
Arthritic Joints
Osteoarthritis
Some Osteonecrosis
Information
http://www.prolotherapy.com/PPM_JanFeb2008_Crane_PRP.pdf
https://drjamesbaum.com/wp-content/uploads/stemcells2002-0109.pdf
Important Videos Everyone Should watch on Biologics
https://drjamesbaum.com/2013/07/the-science-of-mesenchymal-stem-cells-and-regenerative-medicine/
Scientific Papers on Research of Stem Cells
https://drjamesbaum.com/stem-cells/scientific-papers/

I will be posting this in my other blog section also